Why Causality of Death Following Vaccination Can No Longer Be Proven: Understanding the WHO’s 2019 AEFI Framework
The 2019 WHO AEFI (Adverse Event Following Immunization) Framework raised the evidentiary threshold so high that proving vaccine-related injury or death has become practically impossible.
Preface
It is well known that WHO’s agenda is heavily shaped by private and corporate-linked donors—most notably the Gates Foundation, Gavi, and pharmaceutical-sector partners—because over 80% of its budget consists of earmarked funds tied to donor-defined priorities.
Not surprisingly, WHO-developed guidelines and policies are driven by interests of its donors much more than by interests of Canadians. A clear example of this is the 2019 WHO AEFI framework, which raised the evidentiary threshold for vaccine-related injury and death so high that it has become practically impossible to attribute serious reactions—including deaths—to vaccination.
Under this new framework, Canadians cannot formally prove causality in cases where it previously would have been possible, even in well-documented tragedies such as the death of a young hockey player, Sean Hartman. The practical effect is to shield vaccine-investing corporations from enormous financial exposure, while families are left without recognition or recourse.
The union responsible for defending its members must be fully aware of this situation. Without that awareness, it cannot adequately support affected members or challenge employer policies that may be shaped by external corporate interests rather than by the wellbeing of Canadians.
This is why, in line with my efforts to provide evidence of political interference in health policies begun in my previous articles, I have now created a new page on my portal dedicated to gathering evidence of external, big-pharma–driven influence on Canadian health policies. This article begins that collection.
Analysis of harmful WHO interference in Canadian public health policy
This analysis began with publicly available federal data from https://health-infobase.canada.ca/.
Thanks to the Open Canada initiative, this portal allows citizens, researchers, and public servants to quickly locate vital information, including statistics on deaths reported following COVID-19 vaccination. It was in reviewing those numbers that I discovered a profound disconnect between the raw data and the final causality conclusions. That discovery led directly to the 2019 WHO AEFI causality framework—the topic of this article.
In the article that follows, I show that the WHO’s revised methodology makes it extraordinarily difficult, in practice, to establish whether a death occurring shortly after vaccination was caused by the vaccine. This is not a technical detail. It affects real Canadian families, many of whom have faced sudden tragedy without the ability to obtain clear answers or recognition—despite compelling timelines, the absence of prior health conditions, and even in cases where biological evidence was obtained outside Canada at personal expense.
In another article, I presented evidence from another federal report related to the post-marketing evaluation of COVID-19 vaccine effectiveness. That analysis highlighted a separate concern: the significant overstating of vaccine benefits through a distorted interpretation of “cases following vaccination” data, which was heavily skewed to reinforce foreign corporate interests’ messaging on vaccine efficacy.
Together, these investigations form a broader effort to document how foreign corporate interests interfered with and harmed Canadian health-policy decision-making.
Source:
https://health-infobase.canada.ca (Search “COVID”)
Reported side effects following COVID-19 vaccination in Canada
Data exploration tool, COVID-19, Vaccines, Number of reported adverse events following immunization against COVID-19. Last updated: 2023-09-29
WHO guidance on causality assessment specific to vaccinations: Causality assessment of an adverse event following immunization (AEFI): user manual for the revised WHO classification, 2nd ed., 2019 update, 16 April 2021 | Manual (88 pages): https://www.who.int/publications/i/item/9789241516990
Contents:
Main Article (also published at https://en.gorodnichy.ca/evidence/big-pharma-influence)
Appendix A: Itemized highlights and direct quotations from the 2019 WHO AEFI Causality Assessment User Manual,
Appendix B: Historical Evolution of AEFI Causality Methods
Related articles:
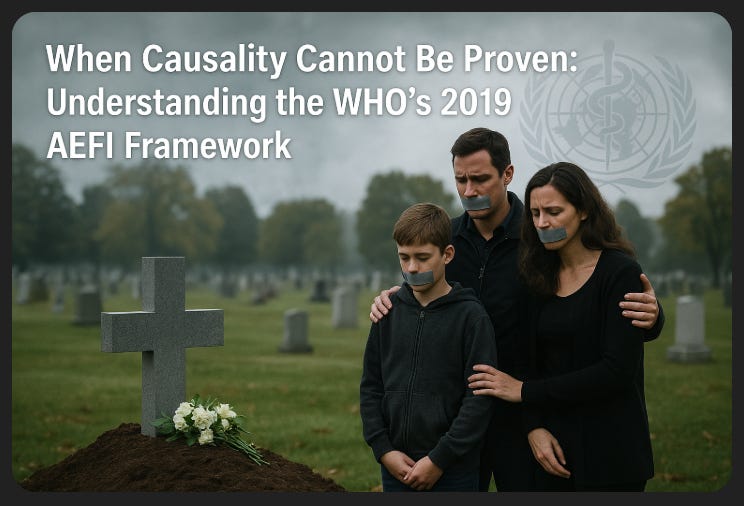
When Causality Cannot Be Proven: Understanding the WHO’s 2019 AEFI Framework
Introduction
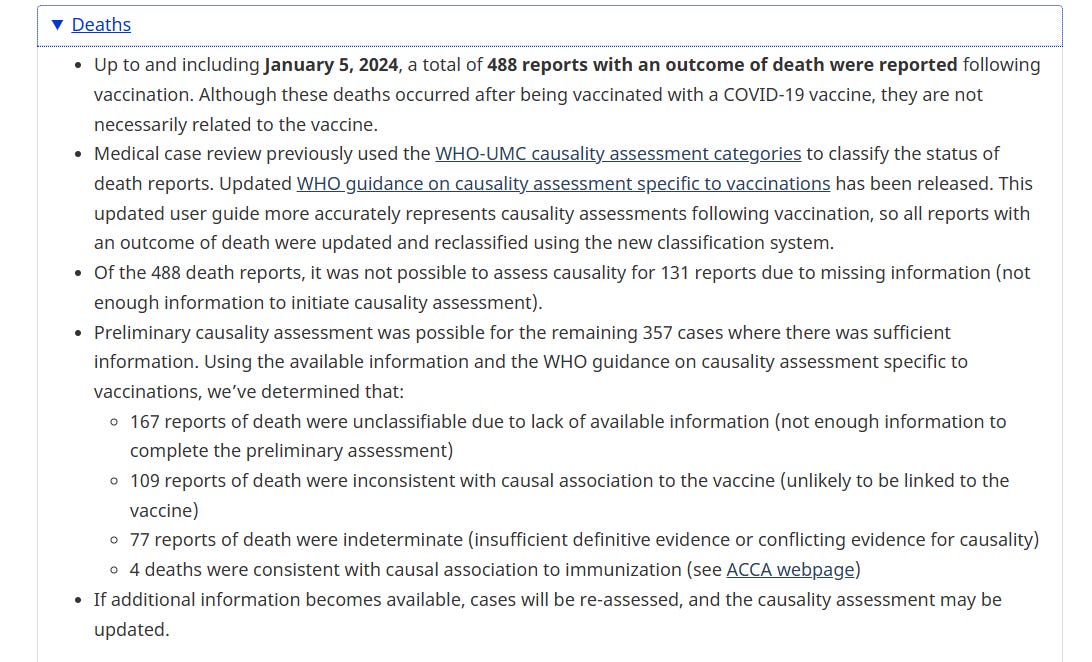
Across Canada, many families have attempted to navigate the federal system for reporting adverse events following COVID-19 vaccination. They rely on federal data, including the Reported Side Effects Following COVID-19 Vaccination in Canada dashboard, last updated on 29 September 2023. That dashboard reports 488 deaths occurring after COVID-19 vaccination. Yet only four of those were ultimately classified as “consistent with causal association to immunization”.
The central question for Canadians—especially for public servants, union members, and those affected by mandatory workplace vaccination policies—is this:
How did 488 post-vaccination deaths result in only 4 causally associated cases?
The answer lies in the 2019 revised WHO guidance on causality assessment of AEFI (Adverse Event Following Immunization). This 88-page manual created a new methodology, new terminology, and new evidentiary thresholds that countries—including Canada—have since adopted. The manual is attached here for reference.
This article explains, in clear and policy-neutral terms, how these new guidelines function, why they make causality extremely difficult to establish, and how this affects families such as the Hartman family—whose teenage son Sean died shortly after mandatory vaccination, yet the causality ruling could not be obtained.
This analysis is not an attack on health authorities. Rather, it is a call for transparency, understanding, and informed debate—values central to a healthy public service.
Fact Under Investigation: Of 488 Post-Vaccination Deaths, Only 4 Causally Linked
On the Government of Canada’s official COVID-19 vaccine safety page, we read the following:
“Up to and including January 5, 2024, a total of 488 reports with an outcome of death were reported following vaccination … Using the available information and the WHO guidance on causality assessment specific to vaccinations, we’ve determined that … 4 deaths were consistent with causal association to immunization.” (health-infobase.canada.ca)
In other words: among 488 deaths that occurred after COVID-19 vaccination, only 4 are officially recognized as “consistent with causal association to immunization” in Canada.
This outcome is not the result of negligence or misconduct. It is the direct, predictable outcome of applying the WHO 2019 causality framework, which requires a very high, often practically unreachable level of evidence before causality can be confirmed.
2. What changed with the WHO’s 2019 AEFI manual
The WHO’s 2019 update presents itself as a technical improvement: a “systematic, standardized global causality assessment process” for serious adverse events following immunization.
The document explicitly states:
that an AEFI is any medical event following vaccination, “which does not necessarily have a causal relationship with the use of the vaccine”;
that causality assessment “usually will not prove or disprove an association” for an individual event, but only estimate a level of certainty;
and that with inadequate or incomplete data, a case may be considered “ineligible” for assessment or “unclassifiable”.
The 2019 update highlights several changes:
“Greater clarity on AEFI cases ineligible for classification and unclassifiable cases”
“Use of clearer language and semantics in the checklist questions”
“Better graphics in the algorithm with emphasis on the mandatory path”
On paper, these sound like neutral technical refinements. But when you look at how the algorithm operates, especially at the individual case level, several structural features make it very difficult for any post-vaccine death to be categorized as “consistent with causal association”:
Strong emphasis on alternative explanations.
Assessors are explicitly instructed to search systematically for other factors: pre-existing conditions, emerging illnesses, coincidental infections, prior trauma, genetic predispositions, other exposures, etc. A “coincidental event” is defined as one caused by “something other than the vaccine product, immunization error or immunization anxiety.”High documentation burden on families and clinicians.
The manual stresses that causality assessment depends heavily on the “availability of adequate medical and laboratory services and access to background information.” With inadequate or incomplete data, a case is simply ineligible or unclassifiable.Temporal proximity alone is not enough.
The document explicitly cautions that the fact that an event follows a vaccine in time “does not automatically suggest that the vaccine caused or contributed to the event.” Even when the timing is highly suggestive (e.g., sudden death shortly after vaccination), the algorithm still requires additional evidence that, in practice, is very hard to obtain.Population-level evidence is given priority over individual plausibility.
The manual stresses that causal links are ideally established at the population level, and that when such population-level evidence is unclear or negative, individual cases tend to be classified as indeterminate or inconsistent with causality.
Taken together, this means:
It is relatively easy for an assessor to conclude that a case is coincidental, indeterminate, or unclassifiable,
and very hard—especially under normal real-world constraints of time, access, and resources—for a grieving family and busy clinicians to assemble the kind of evidence required to reach the category “consistent with causal association to immunization.”
3. How this plays out in Canada’s official data
The Canadian COVID-19 vaccine safety report on Health-Infobase explicitly notes that its death classifications are based on the updated WHO guidance on causality assessment specific to vaccinations. (health-infobase.canada.ca)
Out of 488 reported deaths following COVID-19 vaccination:
131: no assessment was possible due to missing information.
167: “unclassifiable” due to lack of sufficient information to complete the assessment.
109: “inconsistent with causal association to the vaccine” (treated as coincidental).
77: “indeterminate” (insufficient or conflicting evidence).
4: “consistent with causal association to immunization.” (health-infobase.canada.ca)
From a human point of view, this raises obvious questions:
How many of those 131 + 167 = 298 “no information” or “unclassifiable” cases involve families who were simply unable—emotionally, financially, or logistically—to gather the documentation required by the WHO algorithm?
How often are front-line doctors able, in the midst of overloaded practices and complex care demands, to systematically pursue every laboratory investigation, specialist report, and follow-up interview that the framework implicitly expects?
How many cases end up in the “indeterminate” bucket not because the temporal link and clinical picture are weak, but because the paper trail is incomplete?
Officially, we are told that:
“Although these deaths occurred after being vaccinated with a COVID-19 vaccine, they are not necessarily related to the vaccine.” (health-infobase.canada.ca)
Strictly speaking, that statement is true. The problem is what it leaves unsaid:
It does not describe how demanding the WHO-based framework has become for anyone trying to demonstrate causality.
It does not acknowledge how much depends on the capacity and persistence of families and clinicians—people who are often in shock, grief, or burnout.
It does not tell you that the same WHO manual explicitly says that causality assessment “usually will not prove or disprove an association” at the individual level.
For union members and public servants who believe in evidence-based policy, this raises a serious concern: if our global and national systems are designed in such a way that only a tiny fraction of post-vaccine deaths can ever be “proven”, then our official statistics will inevitably under-represent real-world harm.
4. A concrete example: the case of Sean Hartman
To understand what this looks like in real life, consider the widely publicized case of Sean Hartman, a 17-year-old hockey player from Beeton, Ontario.
According to media reports and public testimony:
Sean received a Pfizer-BioNTech COVID-19 vaccine dose in August 2021 in order to comply with league requirements to continue playing hockey.
He died suddenly on September 27, 2021, a few weeks after the shot. He had been previously healthy. (Rebel News)
His father, Dan Hartman, became an outspoken advocate, testifying at public inquiries and interviews about his son’s death and his belief that it was linked to the vaccine. (Facebook)
Because he could not get certain tests done in Canada, Sean’s father reportedly arranged for tissue samples to be analyzed in the United States, including by American pathologist Dr. Ryan Cole, who reported the presence of spike protein in Sean’s tissue. (sandrafinley.ca)
From a layperson’s perspective, the picture looks compelling:
a previously healthy teenager,
pressured into vaccination to participate in normal social life,
who dies shortly thereafter,
with a pathologist reporting spike protein in his tissue.
For many Canadians, including those of us working inside government, this looks like the kind of case where the system should at least recognize a probable vaccine-related causation and trigger a thorough, transparent investigation.
Instead, what happened?
4.1 The legal case and its outcome
Dan Hartman brought a wrongful death lawsuit against Health Canada and Pfizer, arguing that they failed to adequately warn about risks and that Sean’s death was caused by the vaccine. According to coverage of the ruling by outlets such as Blacklock’s Reporter, the Western Standard and Rebel News, an Ontario Superior Court judge dismissed the case in early 2025. (Western Standard)
Key points reported from the decision include:
The court accepted that Sean’s death was tragic but found that the legal test for causation and government liability had not been met.
The judge highlighted that federal health authorities owe a duty to Canadians in general, not to specific individuals, and that the plaintiff had not established that Health Canada failed in a legally actionable way to warn of specific risks. (Rebel News)
The decision did not conclusively state that the vaccine played no role, but effectively determined that the evidence presented was insufficient to meet the legal standard of proof required to hold the defendants liable.
In other words, even in a highly documented, high-profile case—with temporal proximity, a previously healthy youth, and additional pathology testing—the court found that causation could not be legally established.
While the judgment is a legal decision, not a WHO causality assessment, it is operating in the same conceptual environment: an environment where “correlation is not causation,” where alternative explanations must be exhaustively excluded, and where the burden of proof is placed squarely on the grieving family.
4.2 How this connects to the WHO AEFI framework
The WHO manual explicitly instructs assessors to:
treat temporal proximity as necessary but never sufficient;
systematically search for alternative explanations (pre-existing or emerging conditions, infections, spontaneous events, etc.);
classify cases as “indeterminate”, “inconsistent with causal association”, or “unclassifiable” when evidence is incomplete or ambiguous;
and recognize that, in most individual cases, a definite causal association cannot be established.
When you apply this lens to Sean’s case, even with the extra efforts undertaken by his father:
Any undocumented or not fully investigated factor can be treated as a potential alternative explanation.
The presence of spike protein, while suggestive, may be argued over in terms of methodology, background rates, or competing interpretations.
If any element is considered uncertain or incomplete, the case can be placed into “indeterminate” or “inconsistent” categories.
From a technical standpoint, the system is designed to err on the side of classifying such deaths as not clearly vaccine-caused unless the evidence reaches a very high, often unattainable, threshold.
From a human standpoint, especially for those of us in unions and the public service, this means that even a family as determined and resourceful as the Hartmans—who fought for years, traveled across borders, and took on enormous emotional and financial burdens—could not achieve formal recognition of causality, either medically or legally.
5. How many families will never be heard?
The Hartman case is visible because the father was persistent, articulate, and able to pursue legal action and independent testing. But we have to ask:
How many other families experienced the sudden, unexplained death of a loved one after vaccination—
who did not know how to navigate AEFI reporting,
who could not afford independent pathology or cross-border testing,
or who simply did not have the emotional strength to turn their grief into a multi-year battle?
Among the 488 reported deaths in Canada and the unknown number of deaths that were never reported as AEFI at all, how many would have looked like Sean’s story if you sat at their kitchen tables and listened?
Given the structure of the WHO AEFI framework and the reality of clinical practice:
It is statistically unsurprising that only 4 cases out of 488 could be classified as “consistent with causal association.”
It is not an automatic proof that only four people in Canada died because of the vaccine.
Instead, it reflects a system in which only the tiniest fraction of tragedies can ever make it over the bar set by the classification algorithm and, in parallel, by legal standards of proof.
The result is a form of institutionalized silence:
Families who suspect a link are told, in effect, that there is “not enough evidence.”
Doctors are constrained by guidelines that push them toward caution in attributing causality.
Official statistics present a reassuringly low number of “vaccine-related deaths,” which then reinforce policies and mandates.
Unions and public servants, relying on official data, may underestimate the magnitude of harm experienced by a small but real subset of our colleagues and fellow citizens.
Hundreds — and very possibly thousands — of parents and spouses worldwide now live with this double burden: not only the sudden, devastating loss of a loved one, but also a system that tells them it is **“indeterminate,” “coincidental,” or “unclassifiable.” Their stories rarely make it into court decisions or official reports. Most of them will remain unheard.
6. What unions and public servants can do
As union members and public servants, we cannot rewrite the WHO manual on our own. But we can:
Acknowledge the structural bias built into current causality frameworks.
Recognize that the 2019 WHO update, while framed as a technical improvement, has the practical effect of making official recognition of vaccine-associated deaths extremely rare.Advocate for independent, transparent reviews of post-vaccine deaths.
Unions can demand that in cases like Sean Hartman’s, families be offered full, independent coroners’ inquests with transparent publication of evidence, rather than being left to fight alone.Support members who are navigating AEFI processes.
Provide guidance on how to document events.
Encourage early reporting.
Help members access medical records and legal advice.
Insist on honesty in risk communication.
Public communications should be clear that:causality assessment frameworks are conservative and often inconclusive at the individual level;
“not proven” is not the same as “definitely not caused by the vaccine”;
a very small number of officially recognized deaths does not automatically mean that harms are negligible.
Promote a culture of empathy rather than dismissal.
Whether or not a case meets the technical threshold set by WHO, families like the Hartmans should not be treated as “misinformed” or “anti-science,” but as citizens whose lived experience points to gaps in our systems.
7. Conclusion: recognition as a form of justice
The WHO’s 2019 AEFI causality manual and Canada’s adoption of its framework have created a system where:
almost any alternative explanation can be used to avoid recognizing a death as vaccine-related;
incomplete documentation is enough to classify a case as “unclassifiable”; and
even clear, temporally linked, medically investigated cases can struggle to be acknowledged as “consistent with causal association to immunization.”
In that system, only 4 out of 488 reported post-vaccine deaths in Canada are officially recognized as causally linked to COVID-19 vaccination. (health-infobase.canada.ca)
The story of Sean Hartman shows what this means in human terms: a healthy young hockey player, a sudden death after a mandated shot, a father who did everything he could—including sending tissue samples to another country—and still could not secure formal recognition of causality in court or in the official safety statistics. (Rebel News)
Behind Sean’s story, there may be hundreds or thousands of similar families around the world: parents who never had the resources to launch a lawsuit, who never found an independent pathologist, who simply collapsed under the weight of grief and bureaucracy. For most of them, their child’s or spouse’s death will remain an “indeterminate event” in a database, or will never be recorded as an AEFI at all.
As public servants and union members, we cannot bring these loved ones back. But we can refuse to let their experiences be erased by classification systems that are too rigid, too demanding, and too far removed from real life.
Recognition is not only a scientific question. It is also a question of justice.
References
Public Health Agency of Canada. COVID-19 vaccine safety: Reported side effects following COVID-19 vaccination in Canada. Government of Canada, updated January 2024. (health-infobase.canada.ca)
World Health Organization. Causality assessment of an adverse event following immunization (AEFI): user manual for the revised WHO classification, 2nd ed., 2019 update. Geneva: WHO; 2019.
Public reports and testimony by Dan Hartman regarding the death of his son, Sean Hartman, including media coverage and inquiry testimony. (Facebook)
Reporting on the Ontario Superior Court decision dismissing the Hartman family’s wrongful death lawsuit regarding Sean’s death following COVID-19 vaccination. (Western Standard)
Council for International Organizations of Medical Sciences (CIOMS) / WHO Working Group. Definition and application of terms for vaccine pharmacovigilance. 2012.
Acknowledgment
This article was written with assistance from ChatGPT using the prompt:
“Write a WA (Write Article) piece for my DG4VP Substack to explain and critically examine the WHO 2019 ‘Causality assessment of an adverse event following immunization (AEFI)’ manual, using Canada’s official Health-Infobase data on 488 reported deaths following COVID-19 vaccination (of which only 4 are classified as ‘consistent with causal association to immunization’). Show how the updated WHO framework makes it extremely difficult—under normal workload conditions for families and doctors—to prove that a death that occurs after a shot was caused by the shot. Explain the technical categories (‘unclassifiable’, ‘indeterminate’, ‘inconsistent with causal association’) and how they map onto real-life barriers for grieving families. Integrate Canada’s official wording and category counts from the vaccine safety report. Then expand the article to include the concrete example of the tragic death of young hockey player Sean Hartman: a previously healthy child who died shortly after COVID-19 vaccination, whose father pursued independent pathology (including spike-protein testing in the U.S.) and brought a wrongful death lawsuit against Health Canada and Pfizer, but still lost his case because causation could not be ‘proven’ under the new framework and legal standards. Use this case to illustrate how even in the clearest and most documented scenarios, the system can still deny formal recognition of vaccine causality, leaving families to suffer in silence. Conclude by reflecting on how many other parents and families may be in similar situations, unable to collect all the paperwork or evidence required, and whose stories will never be heard. The audience is Canadian union members and public servants, and the tone should be factual, respectful, and aligned with the Public Service Code of Values and Ethics.”
Based on approximately 20–30 minutes of narrated input and collaborative drafting with the author.
ChatGPT was also used to ensure political neutrality, factual accuracy, and alignment with the Public Servant Code of Values and Ethics.
Read more about why and how I use ChatGPT to write my Substack articles here.
Support this work across all channels
If you believe in open dialogue, informed choice, and exploring underreported perspectives, help keep the conversation going—like and share this article on your preferred platform.
I write these articles on my own time as a contribution to my community—especially for those seeking truth and guidance in these increasingly censored times. Your support—through follows, likes, and shares—makes a real difference.
You can follow me here:
LinkedIn – https://www.linkedin.com/in/dmitry-gorodnichy/
Facebook – https://www.facebook.com/dmitry.o.gorodnichy/
Twitter/X – https://x.com/Gorodnichy_Dm
YouTube (@Dr.Dmitry.Gorodnichy) – https://www.youtube.com/@Dr.Dmitry.Gorodnichy
YouTube (@IVIM) – https://www.youtube.com/@IVIM
My articles are, and will always remain, free to read.
APPENDIX A: Key Highlights and Quotations from the 2019 WHO AEFI Manual
1. Purpose and Scope of the Framework
Summary:
The WHO states that its AEFI manual provides a standardized global method for assessing causality of adverse events following vaccination. It is written for national and sub-national AEFI committees and immunization program managers.
Key Quote:
“This user manual serves as a guide to a systematic, standardized global causality assessment process for individual serious adverse events following immunization (AEFI). It is intended to be used by staff at national level… and others.”
2. What Changed in the 2019 Update
Summary:
The 2019 update introduces key changes toward greater clarity and stricter classification, especially regarding what counts as “ineligible” or “unclassifiable.” It also introduces expanded guidance on anxiety-related events and consideration of falsified vaccines.
Key Quotes:
New elements include:
“Greater clarity on ‘AEFI cases ineligible for classification’ and ‘unclassifiable cases’…
A broader consideration on… stress responses…
Attention to ‘falsified vaccines’…
Use of clearer language…
Better graphics…
Updated examples…”
This section is crucial, because “ineligible” and “unclassifiable” categories are the core mechanisms by which many cases—despite strong circumstantial evidence—never reach a causal conclusion.
3. Definitions That Shape Causality Assessment
3.1. Adverse Event Following Immunization (AEFI)
Summary:
AEFI does not mean something caused by a vaccine. It merely means something that happened after vaccination.
Quote:
“Any untoward medical occurrence which follows immunization and which does not necessarily have a causal relationship with the usage of the vaccine.”
This definition allows broad inclusion of events while simultaneously allowing most of them to be later excluded from causality.
3.2. Coincidental Events
Summary:
Events that are attributed to anything other than the vaccine are automatically considered “coincidental.”
Quote:
“An AEFI that is caused by something other than the vaccine product, immunization error or immunization anxiety.”
This definition is important because, in practice, when causality cannot be proven to a high standard, cases are defaulted into this “coincidental” category.
4. The Most Consequential Category: “Ineligible” and “Unclassifiable Cases”
Summary:
The manual states that a case can be declared ineligible when insufficient information is available even to form a causality question.
It can be declared unclassifiable when a causality question can be formed but key evidence is missing.
The key issue: most families cannot access advanced lab testing, autopsy data, or specialized diagnostics, resulting in a large number of cases being placed into these categories—even when timing, symptoms, and clinical course strongly suggest a causal link.
Key Quotes:
Ineligible cases
“Cases ineligible for causality assessment are those where the amount of information available to the assessor is limited such that a causality question cannot be created.”
Unclassifiable cases
“Unclassifiable cases occur… when… some important elements are missing to enable a logical classification.”
Instruction to hold and re-attempt later
“It is important to specify the missing elements and make attempts to obtain the information so that causality assessment could be attempted again.”
In practice, however, once an investigation is closed or ruled unclassifiable, families rarely receive further support to pursue new evidence.
5. Guidance Emphasizing Non-Attribution Without Definitive Evidence
Summary:
The WHO explicitly warns against attributing an adverse event to vaccination when information is incomplete, emphasizing that only “adequate information” justifies a causal link.
Key Quote:
“An AEFI should not be causally linked to a vaccine without adequate information.”
This protective standard makes it far easier to rule against causality than to confirm it.
6. Human Factors and the Role of Expertise
Summary:
Causality assessment is framed as a clinical differential diagnosis, requiring advanced experience, expertise, and resources.
Quote:
“The human elements of experience, proficiency, resources and teamwork clearly play an important role.”
Families without access to specialists or forensic expertise—especially in countries where certain tests are not available—are disproportionately disadvantaged by this requirement.
7. Classification Flexibility and Re-classification
Summary:
Cases can move between categories if new evidence becomes available, but only if someone is able to obtain that new evidence—often unrealistic for ordinary citizens.
Quote:
“If additional information becomes available, the classification can move into a more definitive category… reviewers should clarify what additional information would be helpful…”
This re-classification window sounds reassuring but is rarely achievable for grieving families.
8. Instructions on Communicating “Coincidental” Decisions to Families
Summary:
The manual instructs healthcare systems to communicate coincidental findings to families and communities.
Quote:
“The information and confirmation should be provided to patients, their relatives, the care provider and the community.”
However, the manual does not include any mechanism for supporting families who disagree with the conclusion or who cannot obtain the missing evidence.
9. Emphasis on Not Using Limited Information to Attribute Causality
Summary:
This is one of the most powerful statements in the manual, as it sets the threshold for proving causality very high.
Quote:
“A good clinician does not diagnose diabetes or coronary artery disease on the basis of conflicting or vague information. In the same way, an AEFI should not be causally linked to a vaccine without adequate information.”
This reinforces why so many cases—despite clear temporal association and the absence of prior health issues—are still deemed “not causally related.”
APPENDIX SUMMARY — What This Means in Practice
Based strictly on the WHO’s own text, the structure of the 2019 framework shows:
1. A default presumption of non-causality unless evidence is complete and definitive.
Even obvious temporal associations are insufficient.
2. Two large categories—Ineligible and Unclassifiable—absorb most cases lacking complete clinical data.
These categories prevent a causal classification even when parents, clinicians, and timing strongly suggest otherwise.
3. The requirement for “adequate information” sets a bar that most families cannot meet.
4. The system is highly dependent on expert resources that many countries (including Canada) cannot provide for individual families.
5. Re-classification is possible only if new evidence emerges, which is often unattainable.
Appendix B: Historical Evolution of AEFI Causality Methods
Before the 2019 WHO AEFI framework, countries relied on a series of earlier systems for assessing adverse events following immunization. Understanding these predecessors helps explain how the standard of evidence has shifted over time—from a more flexible clinical-judgment model toward today’s highly structured and restrictive algorithm.
1. Pre-2005: WHO–UMC General Pharmacovigilance Categories
For several decades, vaccine-related AEFIs were assessed using the general WHO–UMC drug causality system. Cases were placed into broad categories such as certain, probable, possible, unlikely, conditional/unclassified, or unassessable.
This system relied heavily on clinical judgment, not algorithmic gates, and allowed temporal association and biological plausibility to carry significant weight.
2. 2005: WHO AEFI Causality Aide-Mémoire
In 2005, WHO issued its first dedicated guidance for AEFI investigations, the AEFI Causality Assessment Aide-Mémoire.
This document encouraged national programs to classify AEFIs using a structured but still relatively clinician-driven approach. The emphasis remained on contextual assessment, proximity in time, and differential diagnosis—without the stringent “ineligible/unclassifiable” categories that dominate the current method.
3. 2012: CIOMS/WHO Working Group on Vaccine Pharmacovigilance
A turning point came in 2012, when CIOMS and WHO published a joint report formalizing precise definitions and standardized terminology for vaccine safety.
This report influenced all later frameworks by promoting more uniform, globally aligned analysis, and explicitly redefining concepts such as “coincidental AEFI” and “vaccine product–related reactions.”
4. 2013: WHO AEFI Manual (1st Edition of Revised Classification)
The 2013 manual replaced the WHO–UMC “drug causality” categories for vaccine events, introducing four new AEFI outcomes:
Consistent with causal association
Inconsistent with causal association
Indeterminate
Unclassifiable
This was a significant methodological shift. While temporal association still played a role, the framework required a more systematic process for ruling out alternative causes. Importantly, this was the first appearance of major exclusion categories that could prevent cases from ever reaching causality assessment.
5. 2019: WHO AEFI Manual (2nd Edition, Updated Framework)
The 2019 update—now the global standard—further tightened the structure of AEFI assessment.
Key changes included:
Clearer and expanded definitions of “ineligible” and “unclassifiable” cases, increasing the likelihood that cases lacking full documentation would be excluded.
Greater emphasis on non-vaccine causes, including stress responses and background rates of illness.
Introduction of more formalized graphical algorithms and step-based decision gates.
An explicit warning that causality “should not be linked without adequate information”, shifting the evidentiary burden toward near-certainty rather than clinical plausibility.
With these refinements, the framework became far more conservative in assigning causality—effectively requiring families and clinicians to produce comprehensive, often specialized medical evidence that is rarely obtainable in real-world scenarios.
Summary
From the 1970s to the early 2000s, AEFI analysis relied primarily on expert clinical judgment, flexible evaluation of temporal relationships, and open consideration of biological plausibility.
Between 2012 and 2019, WHO guidance shifted toward a rigid, documentation-heavy, exclusion-first model, culminating in the current system in which the majority of reported cases are categorized as “ineligible,” “unclassifiable,” “inconsistent,” or “indeterminate.”
The 2019 manual therefore represents not simply an update but a fundamental methodological transformation—one that has had far-reaching implications for families seeking recognition of vaccine-related harm.
Appendix C: Earlier version of the article prepared by ChatGPT
TITLE OPTIONS
How the 2019 WHO Causality Guidelines Redefined Vaccine-Related Death Investigations
When Causality Cannot Be Proven: Understanding the WHO’s 2019 AEFI Framework
Why Only Four COVID-19 Vaccine Deaths Were Classified as “Causally Linked”: A Policy Analysis
SUBTITLE OPTIONS
Why the revised WHO methodology makes it extremely difficult for affected families to obtain causality findings—especially during high-volume vaccination campaigns.
Understanding how new international guidance changed the evidentiary threshold for vaccine-related injury and death investigations in Canada.
A data-informed review of the WHO’s AEFI framework and its impact on transparency, accountability, and trust in public health.
ARTICLE (WA FORMAT)
Introduction
Across Canada, many families have attempted to navigate the federal system for reporting adverse events following COVID-19 vaccination. They rely on federal data, including the Reported Side Effects Following COVID-19 Vaccination in Canada dashboard, last updated on 29 September 2023. That dashboard reports 488 deaths occurring after COVID-19 vaccination. Yet only four of those were ultimately classified as “consistent with causal association to immunization”.
The central question for Canadians—especially for public servants, union members, and those affected by mandatory workplace vaccination policies—is this:
How did 488 post-vaccination deaths result in only 4 causally associated cases?
The answer lies in the 2019 revised WHO guidance on causality assessment of AEFI (Adverse Event Following Immunization). This 88-page manual created a new methodology, new terminology, and new evidentiary thresholds that countries—including Canada—have since adopted. The manual is attached here for reference.
This article explains, in clear and policy-neutral terms, how these new guidelines function, why they make causality extremely difficult to establish, and how this affects families such as the Hartman family—whose teenage son Sean died shortly after mandatory vaccination, yet the causality ruling could not be obtained.
This analysis is not an attack on health authorities. Rather, it is a call for transparency, understanding, and informed debate—values central to a healthy public service.
1. The Federal Data: 488 Post-Vaccination Deaths, Only 4 Causally Linked
According to the Public Health Agency of Canada:
488 deaths were reported following COVID-19 vaccination
131 could not be assessed due to missing information
357 had enough information for preliminary assessment
167 were “unclassifiable” (insufficient data)
109 were deemed “inconsistent with causal association”
77 were “indeterminate”
4 were “consistent with causal association to immunization”
In other words:
484 of 488 deaths were excluded from causal association, largely due to lack of information or lack of definitive proof.
This outcome is not the result of negligence or misconduct. It is the direct, predictable outcome of applying the WHO 2019 causality framework, which requires a very high, often practically unreachable level of evidence before causality can be confirmed.
2. The 2019 WHO AEFI Manual: A New Evidentiary Standard
The WHO manual (Second edition, 2019 update) replaced the earlier WHO-UMC system with a more rigid and algorithmic process. It introduced:
Mandatory multi-step eligibility gates
Strict definitions for “valid diagnosis”
High documentation requirements
An expanded list of reasons an AEFI cannot be classified
New emphasis on “stress responses,” “coincidental events,” and “other underlying causes”
The manual repeatedly states that:
“Causality assessment usually will not prove or disprove an association… A definite causal association often cannot be established.”
This is a foundational assumption of the system. Under the 2019 rules, causality becomes the exception—not the default possibility.
3. Why It Becomes Almost Impossible for Families to Prove Causality
The revised framework includes four major structural barriers:
Barrier 1: Missing paperwork = case cannot be assessed
If any required piece of medical information is incomplete, unavailable, or lost—especially during emergency clinical care—the case becomes:
“Ineligible” (cannot even begin assessment), or
“Unclassifiable” (assessment started but could not be completed).
This is what happened in 167 of Canada’s death reports.
Families in crisis—especially after sudden death—are rarely in a position to assemble exhaustive medical documentation.
Barrier 2: Every alternative explanation must be ruled out first
The manual requires reviewers to eliminate all other possible causes, even theoretical ones:
pre-existing conditions
undetected infections
spontaneous unrelated events
genetic predispositions
environmental exposures
stress responses
background rates of sudden death
If any plausible alternative exists—even if unproven—the case moves into:
“Inconsistent with causal association”, or
“Indeterminate”
Barrier 3: Temporal proximity is not considered evidence
The updated system explicitly warns that an event occurring shortly after vaccination does not indicate causality.
This directly conflicts with traditional medical logic (post hoc diagnosis) that clinicians use for most other pharmaceutical assessments.
Barrier 4: Definitive proof is almost never available
The manual states that laboratory proof is the only “definitive” evidence, yet:
For COVID-19 vaccines, no such laboratory test exists.
For sudden cardiac events, pulmonary embolism, myocarditis leading to arrhythmia, or autoimmune responses, immediate tissue sampling is rarely possible.
Autopsies—when performed—often cannot determine mechanistic causality.
Thus, the system defaults to “indeterminate.”
4. The Consequence: Why Canada Recorded Only Four Causally Linked Cases
Under the WHO methodology, a death can only be linked to vaccination if all four criteria are satisfied:
No missing information
A valid, precisely defined diagnosis
Strong evidence ruling out all alternative explanations
Strong evidence that the vaccine did cause the event
The vast majority of real-world cases fail step 1 or 3.
Thus, structurally:
The WHO framework makes it extremely difficult—often practically impossible—for individuals or families to obtain a finding of vaccine-related causality.
This explains why families like the Hartmans, despite credible timelines and the absence of alternative explanations, were unable to obtain causality rulings.
5. Why This Matters to Canadian Public Servants and Union Members
Between 2021 and 2022, millions of Canadians—including federal public servants—faced workplace mandates, employment consequences, and social pressure to vaccinate.
When rare adverse events occur, especially in young and previously healthy individuals, affected families expect:
transparent processes
fair evaluations
accessible pathways for review
accountability, where appropriate
However, if the global standard adopted by Canada makes causal confirmation nearly unattainable, families are left without recognition, support, or closure.
For unions and public servants, this raises critical questions about:
equitable treatment of members
access to compensation programs
rights of employees affected by mandated medical interventions
adequacy of information provided before mandates were imposed
long-term policy lessons for future national emergencies
The purpose of this article is not to assign blame, but to ensure that public servants understand the systems governing their rights, risks, and protections.
6. Towards a More Transparent and Supportive Framework
Several reasonable reforms could improve confidence:
Independent AEFI review pathways for mandated populations
Clearer communication to Canadians about how causality assessments actually work
Alternative compensation mechanisms that do not require proof of causality
Regular audits of incomplete or unclassifiable cases
Statutory rights to access all relevant records, including autopsy materials
Union involvement in supporting affected members and families
These reforms would not undermine public health. They would strengthen trust.
Conclusion
The 2019 WHO AEFI causality manual represents a global shift toward an extremely stringent evidentiary framework. Its structure ensures that only the rarest, most clearly documented cases can be classified as causally linked to vaccination.
This explains why, in Canada:
488 reported deaths
resulted in
only 4 cases deemed causally consistent.
For families who lost loved ones shortly after vaccination, this system can feel indistinguishable from systemic dismissal. For public servants and union members, understanding this framework is essential for informed dialogue about rights, accountability, and future emergency policies.
Transparency is not a threat to public health. It is the foundation upon which trust is built.
References
Public Health Agency of Canada. Reported Side Effects Following COVID-19 Vaccination in Canada.
World Health Organization. Causality assessment of an adverse event following immunization (AEFI): user manual for the revised WHO classification, 2nd ed., 2019 update. Geneva: WHO; 2019.
Additional peer-reviewed literature on vaccine safety methodology and AEFI classification.
Disclaimer
This article’s opinions are those of the author and do not represent the views of any Canadian agency, department, university, or organization. It is provided for information and discussion purposes only and does not constitute legal, medical, or professional advice.
Acknowledgment
This article was written with assistance from ChatGPT using the prompt: “Draft a WA-format Substack article for DG4VP analyzing how the 2019 revised WHO causality assessment guidelines (AEFI manual) affect the classification of post-vaccination deaths in Canada, referencing federal data showing 488 reported deaths with only 4 causally associated, explaining why the methodology makes causation nearly impossible to establish, and incorporating attached WHO document content.”
Based on approximately 2,500 words and 25 minutes of narrated input and collaborative drafting with the author.
ChatGPT was also used to ensure political neutrality, factual accuracy, and alignment with the Public Servant Code of Values and Ethics.
Read more about why and how I use ChatGPT to write my Substack articles here.